How Light Fasting Helped Me Catch Health Issues Early — A Real Story
For years, I felt "fine" — until I wasn’t. Minor fatigue, occasional bloating, nothing serious, or so I thought. Then I tried light fasting: skipping meals gently, tuning into my body’s signals. Within weeks, patterns emerged. My energy dipped predictably. My digestion reacted clearly. These weren’t random glitches — they were warnings. Light fasting didn’t cure me, but it woke me up. It gave me a window into my health long before symptoms screamed for attention. What began as a quiet experiment became a lifeline, revealing imbalances I had ignored for years. This is not a miracle cure story. It’s a story about listening — and what happens when we finally do.
The Silent Signals: When “Fine” Isn’t Enough
Many women in their 30s, 40s, and 50s live in a state of "functional fatigue" — getting through the day, managing family, work, and household demands, yet feeling subtly off. They aren’t sick enough to see a doctor, but not quite well either. This in-between space is where early health issues often go unnoticed. Symptoms like afternoon sluggishness, irregular digestion, mild joint discomfort, or trouble sleeping are easily dismissed as part of aging or stress. But these are not normal wear-and-tear signs. They are messages — quiet, persistent signals that something in the body’s balance is shifting.
Modern life makes it easy to ignore these signals. Constant eating, caffeine dependence, packed schedules, and screen-heavy routines dull our ability to sense what the body is trying to communicate. Meals are often eaten on the go, without pause or presence. Hunger and fullness cues get distorted. Over time, we lose touch with our natural rhythms. The body speaks in whispers — a slight heaviness after certain foods, a dip in focus mid-morning, restless nights — but we’ve trained ourselves not to listen. The danger lies in this disconnect. By the time symptoms become loud — chronic fatigue, weight gain, high blood pressure — the underlying condition may have progressed silently for years.
Early detection is one of the most powerful tools in preventive health. It allows for gentle, lifestyle-based interventions before medication or more aggressive treatments become necessary. Consider the case of a woman in her early 40s who began noticing that her energy crashed every afternoon, no matter how much coffee she drank. She attributed it to parenting stress. But when she started paying attention during a period of light fasting, she realized the crash followed a predictable pattern — about four hours after eating carbohydrates. This clue led her to request a blood sugar test, which revealed early insulin resistance. With dietary changes and increased movement, she reversed the trend before prediabetes developed. Her story isn’t unique. It illustrates how small shifts in awareness can lead to significant health protection.
What Is Light Fasting — And Why It’s Not a Diet Trend
Light fasting is not about extreme calorie restriction or dramatic weight loss. It is a gentle, intentional pause in eating that allows the body time to rest, reset, and respond. Unlike prolonged fasts that can last days, or aggressive intermittent fasting regimens that compress eating into narrow windows, light fasting is accessible and sustainable. It might mean delaying breakfast until 9 a.m. after an 8 p.m. dinner — creating a 13-hour gap without food. Or it could involve skipping a snack and eating only three balanced meals, with no grazing in between. The core idea is simplicity: give the digestive system a break so the body can shift from "processing" mode to "monitoring" mode.
This shift is supported by science. When the body isn’t busy breaking down food, it can focus on maintenance and repair. One key process is autophagy — a cellular cleanup mechanism where the body removes damaged proteins and recycles old components. While intense fasting can boost autophagy, even mild fasting periods, such as a 12-hour overnight fast, can support this natural renewal process. Another benefit is metabolic switching: after about 10–12 hours without food, the body begins to shift from using glucose as its primary fuel to tapping into stored fat. This transition supports metabolic flexibility — the ability to switch between fuel sources efficiently — which is linked to better energy stability and reduced risk of metabolic disorders.
What sets light fasting apart from diet culture is its purpose. It is not about shrinking the body or chasing a number on the scale. It is about tuning in. The goal is not restriction, but observation. By creating space between meals, you allow physical sensations — hunger, energy, mood, digestion — to surface more clearly. This makes it easier to notice how different foods, stress levels, and sleep patterns affect your well-being. For many women, this practice becomes a form of self-care rather than a challenge. It fosters a deeper relationship with the body, one built on attention rather than control. When done with kindness and consistency, light fasting becomes less about what you’re not eating, and more about what you’re learning.
Tuning In: How Fasting Amplifies Body Awareness
When you remove the constant input of food, your body’s signals become easier to read. Think of it like turning down background noise to hear a quiet voice. During regular eating patterns, especially with frequent snacking, the digestive system is always active. This constant activity can mask subtle cues — a slight inflammation, a blood sugar spike, a delayed stress response. But when you introduce a pause, those signals rise to the surface. You begin to notice when your energy dips, when your mind feels foggy, or when your mood shifts — not in reaction to food, but in response to your body’s internal state.
One of the most immediate effects women report is a clearer sense of true hunger. Without habitual snacking, the body relearns the difference between physical hunger and emotional or habitual eating. This distinction is powerful. It allows you to eat when you’re truly in need, rather than out of boredom, stress, or routine. At the same time, other sensations become more pronounced. Some notice that headaches occur at the same time each day during fasting, which may point to caffeine withdrawal or blood sugar fluctuations. Others observe that joint stiffness improves after longer fasting windows, suggesting a link between eating patterns and inflammation.
Sleep quality often shifts as well. Many women find that finishing dinner earlier and avoiding late-night snacks leads to deeper, more restful sleep. This is not just about digestion — it’s about circadian rhythm alignment. The body’s internal clock is closely tied to eating patterns. When meals are consumed within a consistent window, the body’s natural repair cycles during sleep become more efficient. Over time, this enhanced awareness builds a clearer picture of personal health rhythms. You start to see how stress affects digestion, how hydration influences energy, and how food choices echo through your day. This is not about diagnosing conditions — it’s about gathering information. And that information becomes the foundation for better decisions.
Early Warnings: Recognizing Patterns Before Symptoms Worsen
Light fasting doesn’t create health problems — it reveals them. When the body has time to rest, imbalances that were previously masked by constant eating or stimulants become visible. For example, a woman in her late 40s began a 12-hour nightly fast, eating between 8 a.m. and 8 p.m. After two weeks, she noticed that she felt unusually fatigued by mid-afternoon, even after a good night’s sleep and a nutritious breakfast. This wasn’t normal for her. She also experienced mild dizziness when standing up quickly. Concerned, she tracked her symptoms and consulted her doctor. Blood tests revealed low iron levels and borderline anemia — issues that had been developing slowly but were now detectable because her body wasn’t relying on constant food intake to prop up energy.
Another common pattern involves digestive discomfort. A woman in her 50s started skipping her evening snack and found that her bloating improved significantly. But she also noticed that certain meals — particularly those high in processed grains — still caused discomfort, even during her eating window. This observation led her to explore food sensitivities, and she eventually discovered she was sensitive to gluten. By adjusting her diet, she reduced inflammation and improved her overall comfort. These examples show how light fasting acts as a mirror — reflecting back what’s already happening inside the body, just more clearly.
Other red flags may include prolonged mental fog, difficulty concentrating during fasting periods, or mood swings that correlate with eating times. These could indicate blood sugar instability, hormonal shifts, or nutrient deficiencies. Headaches that occur regularly at the same time each day during fasting might suggest dehydration, electrolyte imbalance, or caffeine dependence. While none of these symptoms are definitive on their own, their consistency and timing provide valuable clues. The key is not to jump to conclusions, but to use these observations as prompts for further inquiry. When women bring this kind of detailed self-awareness to medical appointments, doctors can make more informed assessments. Early detection means earlier intervention — and often, a better outcome.
A Practical Approach: Starting Light Fasting Safely
Beginning light fasting should be gradual and respectful of your body’s needs. The most accessible starting point is a 12-hour overnight fast. For example, finish dinner by 7 p.m. and wait until 7 a.m. to have breakfast. This simple shift aligns with natural circadian rhythms and requires no drastic changes. As your body adjusts, you can extend the window by 30 to 60 minutes if it feels comfortable. The goal is not to push limits, but to create space for observation. During the fasting period, drink water, herbal tea, or black coffee — liquids without calories that support hydration without breaking the fast.
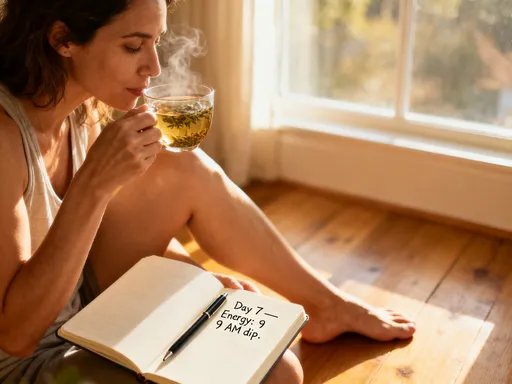
Hydration is essential. Many women mistake thirst for hunger, especially in the early stages. Drinking enough water throughout the day helps stabilize energy and reduces false hunger signals. Keeping a simple journal can also be helpful. Note when you eat, when you feel hungry, your energy levels, sleep quality, and any physical or emotional changes. Over time, patterns will emerge. This record becomes a personal health map, offering insights that numbers on a scale never could.
It’s important to listen to your body. If you feel weak, dizzy, or overly fatigued, shorten the fasting window or pause the practice. Light fasting is not meant to cause distress. Women who are pregnant, breastfeeding, or managing chronic conditions like diabetes, adrenal fatigue, or eating disorders should consult a healthcare provider before beginning. The same applies to those taking medications that affect blood sugar or metabolism. Professional guidance ensures safety and personalization. The aim is not perfection, but awareness — a gentle, sustainable way to reconnect with your body’s wisdom.
Beyond the Fast: Building a Responsive Health Routine
Light fasting is not a standalone solution. Its true value lies in the insights it provides — insights that can shape a more responsive, personalized health routine. Once you begin to recognize patterns, you can make informed choices about food, sleep, movement, and stress management. For example, if you notice that energy dips after eating refined carbohydrates, you might choose more whole grains and balanced meals. If poor sleep follows late dinners, you may decide to eat earlier and create a calming evening routine. These are not rigid rules, but adaptive strategies based on real-time feedback from your body.
Improved sleep often becomes a natural outcome. When the digestive system isn’t working late into the night, the body can focus on repair and restoration. This supports hormonal balance, immune function, and mental clarity. Similarly, reduced stress is a common benefit. As women gain confidence in their ability to interpret bodily signals, they feel more in control of their health. This sense of agency reduces anxiety and promotes emotional well-being. Movement also tends to improve — not through forced exercise, but through a renewed desire to care for the body. A walk after dinner, stretching in the morning, or gentle yoga become natural extensions of a mindful lifestyle.
The shift is from reactive to proactive. Instead of waiting for a crisis to make changes, women begin to act on early cues. They adjust before burnout, modify before imbalance becomes illness, and listen before symptoms escalate. This is the essence of preventive health — not avoiding disease through fear, but cultivating well-being through attention. Light fasting becomes a tool in a larger toolkit: one way to stay connected, informed, and empowered. It’s not about perfection, but about presence. And presence, over time, builds resilience.
Why This Matters: Taking Charge Before Crisis Hits
Health is not merely the absence of disease. It is the presence of balance, energy, and responsiveness. Light fasting, when practiced with care, offers a simple yet profound way to reconnect with that balance. It doesn’t promise dramatic transformations or overnight cures. What it does offer is clarity — a chance to see beneath the surface of daily life and catch subtle shifts before they become serious problems. For women juggling countless responsibilities, this practice is not another burden, but a form of self-respect. It says: I am worth listening to. My body matters. My well-being is a priority.
The stories shared here are not isolated. Thousands of women have discovered similar insights through gentle fasting practices. They haven’t followed extreme protocols or adopted rigid rules. They’ve simply created space to pay attention. And in that space, they’ve found early warnings, made timely changes, and regained a sense of control. This is the power of awareness. It doesn’t require expensive tests or complex interventions. It begins with a pause — a meal delayed, a glass of water, a moment of stillness.
Still, professional medical guidance remains essential. No self-observation replaces a doctor’s expertise. Blood tests, physical exams, and clinical assessments are irreplaceable. But when personal insight and medical care work together, the result is a stronger, more informed approach to health. Light fasting is not a substitute for medicine — it’s a complement. It helps you become an active participant in your care, not just a passive recipient.
In the end, the goal is not to fast forever, but to live better. To make choices that honor your body’s needs. To catch issues early, respond wisely, and maintain vitality through the years. Small, consistent habits — like giving your digestion a break, drinking more water, or noticing how you feel after meals — can have a lasting impact. They build a foundation of health that supports you through every stage of life. And that is a promise worth keeping.