How I Rebuilt My Strength After Surgery — A Real Woman’s Healing Journey
Recovering from surgery or injury is more than physical—it’s emotional, mental, and deeply personal. For women, healing often comes with added pressures to “bounce back” fast. I know because I’ve been there. After my own rehab journey, I learned that true recovery isn’t about speed—it’s about listening to your body, making smart moves, and staying consistent. This is what actually helped me regain strength, confidence, and balance—no hype, just real steps that work.
The Hidden Struggle: Why Women’s Rehab Needs a Closer Look
For many women, the road to recovery after surgery or injury is not just about healing tissue—it’s about navigating a complex web of physical, emotional, and societal expectations. Unlike standardized medical guidelines, the reality of healing is rarely linear. Fatigue lingers long after stitches are removed. Emotional dips—moments of frustration, sadness, or even guilt for not “doing enough”—are common but rarely discussed. These challenges are often compounded by the unspoken pressure to return quickly to caregiving roles, household duties, or professional responsibilities. While men may face similar expectations, women are more likely to internalize them as personal failures if they fall short.
One reason women’s recovery paths differ lies in biological and lifestyle factors. Hormonal fluctuations, particularly in estrogen and progesterone, influence inflammation, pain sensitivity, and tissue repair. These shifts can affect how quickly and comfortably a woman progresses through rehab. Additionally, core strength and pelvic floor integrity—often compromised during pregnancy or certain surgeries—play a critical role in functional recovery. Yet, many standard rehabilitation programs do not address these uniquely female concerns with the depth they require. A one-size-fits-all approach may overlook the importance of rebuilding intra-abdominal pressure control or retraining deep stabilizing muscles.
Lifestyle roles further complicate healing. Women frequently act as the emotional and logistical center of their households. When illness or surgery disrupts this role, the psychological burden can be significant. The desire to resume normal duties quickly may lead to overexertion, which in turn delays healing. This creates a cycle: push too hard, feel worse, feel guilty, then push again. Recognizing this pattern is the first step toward breaking it. The gap between general rehab advice and women-specific needs is real—and closing it begins with acknowledging that recovery is not just physical rehabilitation but holistic restoration.
My Turning Point: From Frustration to Focus
My own journey began after abdominal surgery that, while successful, left me feeling disconnected from my body. At first, I assumed healing would follow a predictable timeline: a few weeks of rest, gradual activity, and then back to life as usual. But reality didn’t cooperate. Weeks turned into months, and I still struggled with low energy, a weakened core, and a persistent fear of movement. Simple tasks like lifting groceries or bending to tie a shoe triggered anxiety. I avoided stairs, dreaded long walks, and felt embarrassed by my limitations. I wasn’t healing the way I thought I should—and that thought weighed heavily on me.
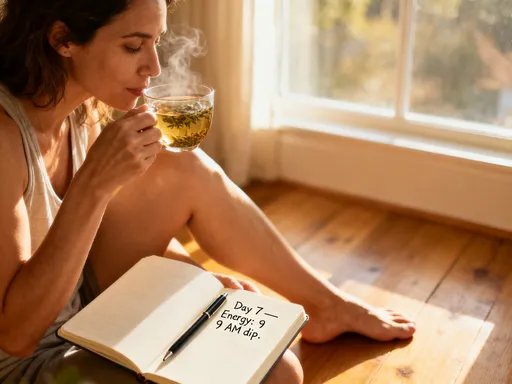
The turning point came on a quiet Tuesday morning. I had tried to do a short home workout, convinced I was “ready,” only to spend the rest of the day in discomfort, mentally berating myself for being “weak.” That night, I sat with my journal and wrote honestly: “I’m not failing because I’m slow. I’m failing because I’m not listening.” That moment of clarity shifted everything. I realized healing wasn’t something that happened to me—it was something I had to actively participate in, with awareness and compassion. I had been treating recovery like a race, measuring progress by how fast I could return to my old routines. But true healing required a different mindset: one rooted in patience, observation, and respect for my body’s signals.
This new perspective didn’t erase the challenges, but it changed how I faced them. Instead of pushing through pain, I began to ask: What is my body trying to tell me? Instead of comparing myself to others, I focused on small, sustainable improvements. Progress, I learned, wasn’t measured in speed but in consistency and self-awareness. The shift wasn’t dramatic—it was subtle, like adjusting the focus on a camera until the image finally came into clear view. From that point forward, I approached recovery not as a problem to be solved, but as a process to be honored.
The Foundation: Listening to Your Body (Not the Clock)
One of the most powerful lessons I learned was that healing begins with listening—not to doctors, apps, or timelines, but to the quiet, consistent voice of the body. “Listening to your body” is often mentioned in wellness circles, but it’s rarely explained in practical terms. It means distinguishing between discomfort, which can be a sign of growth, and pain, which signals harm. It means recognizing fatigue as a cue to rest, not a personal flaw. It involves noticing subtle shifts: a deeper breath, a steadier stance, a moment of ease in a movement that once caused strain. These small signals are the language of healing, and learning to interpret them is essential.
Women, especially those accustomed to managing multiple responsibilities, often override these signals. The habit of “pushing through” becomes second nature—getting through the school run, finishing the work project, attending the family event—regardless of physical cost. This pattern can persist during recovery, where the desire to be “normal” again overrides bodily wisdom. The body may whisper, but the mind shouts: “You should be better by now.” This internal conflict can delay healing by encouraging overexertion on good days and guilt on bad ones. The result is a rollercoaster of progress and setbacks, leaving women feeling confused and discouraged.
Practical tools can help rebuild this lost connection. Daily check-ins take only a few minutes but yield valuable insights. One effective method is the breath-body scan: sitting quietly, placing a hand on the abdomen, and observing the natural rhythm of breathing. Is the breath shallow or deep? Is there tension in the shoulders or jaw? Another approach is movement journaling—recording how specific activities feel, not just what was done. Did walking to the mailbox cause strain? Did stretching ease stiffness? Noting these details creates a feedback loop that fosters awareness. Celebrating small wins—like standing longer in the shower without dizziness—reinforces positive progress and builds confidence over time.
Movement That Heals: Gentle But Effective Strategies
Movement is medicine, but not all movement is created equal—especially during recovery. The key is to engage in activities that support healing without triggering setbacks. This means starting gently, focusing on quality over quantity, and progressing at a pace that respects the body’s current capacity. The goal isn’t to burn calories or build muscle quickly, but to re-establish neuromuscular connections, improve circulation, and restore functional strength. For women rebuilding after surgery, this often means beginning with foundational movements that reignite core stability and joint awareness.
The progression typically follows three phases. The first is breath and activation. Diaphragmatic breathing—deep, slow breaths that expand the belly rather than the chest—triggers the parasympathetic nervous system, reducing stress and improving oxygen flow to healing tissues. This simple practice also engages the transverse abdominis and pelvic floor, two muscle groups often weakened after abdominal or pelvic surgeries. Gentle pelvic tilts, heel slides, and seated marches can further activate these deep stabilizers without strain. These movements may seem too basic to matter, but they lay the groundwork for all future strength.
The second phase introduces supported mobility. Walking is one of the most effective and accessible tools. Starting with short, slow walks—five to ten minutes, two or three times a day—improves circulation, reduces stiffness, and boosts mood. Using a cane or walker when needed is not a sign of weakness but of wisdom. Supported yoga, particularly restorative or chair-based practices, enhances flexibility and body awareness while minimizing joint stress. Poses like supported bridge, seated forward fold, and gentle cat-cow stretch promote mobility without overloading healing tissues. Resistance bands, used with controlled movements, allow for safe strength building. Exercises like banded rows, shoulder presses, and leg abductions can be done seated or standing, with resistance adjusted as strength improves.
The third phase gradually increases load and complexity, but only when earlier stages feel stable. This might include bodyweight squats with support, step-ups using a low platform, or light dumbbell work. The emphasis remains on form, control, and consistency. Rushing into high-intensity workouts or complex movements risks setbacks. Instead, the focus is on building endurance and confidence through repetition and mindful execution. Movement becomes a daily ritual, not a performance.
Fueling Recovery: Nutrition as Support, Not a Diet
Nutrition plays a vital role in healing, yet it’s often misunderstood as a tool for weight control rather than tissue repair. During recovery, the body requires specific nutrients to rebuild collagen, repair muscle, and maintain energy. Protein is essential—it provides the amino acids needed for tissue regeneration. Including a source of high-quality protein in every meal—such as eggs, fish, poultry, beans, or dairy—supports muscle recovery and satiety. Iron, found in leafy greens, lentils, and lean meats, helps maintain energy levels by supporting oxygen transport in the blood. Vitamin C, abundant in citrus fruits, bell peppers, and broccoli, aids collagen formation, which is crucial for wound healing.
Omega-3 fatty acids, present in fatty fish, walnuts, and flaxseeds, help regulate inflammation—a natural part of healing that can become excessive if not balanced. Hydration is equally important; water supports cellular function, nutrient delivery, and joint lubrication. Even mild dehydration can worsen fatigue and slow recovery. Aiming for consistent fluid intake throughout the day—starting with a glass of water upon waking—makes a noticeable difference. These nutrients work best when consumed through whole, minimally processed foods, which also provide fiber, antioxidants, and other co-factors that support overall health.
Emotional and practical challenges often affect eating habits during recovery. Appetite may decrease due to medications, stress, or reduced activity. Conversely, emotional eating—using food for comfort during frustration or boredom—is common. Both responses are normal and do not reflect failure. The goal is not perfection but consistency. Simple strategies can help maintain nourishment without adding stress. Preparing meals in batches when energy allows—such as cooking a large pot of soup or stew—provides ready-to-eat options on low-energy days. Keeping healthy snacks within reach—like yogurt, fruit, or nut butter with apple slices—encourages regular intake. Eating slowly, in a calm environment, improves digestion and satisfaction. Nutrition during recovery is not about restriction or transformation—it’s about giving the body the raw materials it needs to heal.
Mental Reset: Managing the Emotional Side of Healing
Emotional well-being is not a side effect of physical recovery—it is a core component of it. Frustration, impatience, and low mood are common during rehab, especially when progress feels slow or invisible. These feelings are not signs of weakness but natural responses to loss of autonomy, routine disruption, and physical limitation. Ignoring them can create tension that manifests as muscle tightness, sleep disturbances, or increased pain sensitivity. Addressing emotional health is not a distraction from healing; it is a necessary part of the process.
Mindfulness practices offer practical ways to manage these emotions. Spending a few minutes each day focusing on the breath, body sensations, or sounds in the environment helps ground the mind in the present moment. This simple act reduces rumination about the past or anxiety about the future. Guided meditations, available through reputable apps or online platforms, can support this practice without requiring prior experience. Journaling also serves as a valuable outlet—writing about thoughts and feelings can clarify them and reduce their intensity. Reframing goals is another powerful tool. Instead of measuring success by how much activity was completed, shift the focus to how the body felt during and after. Did movement leave you energized or drained? Did rest bring relief? These reflections foster self-compassion and realistic expectations.
Social support plays a crucial role. Sharing struggles with trusted friends or family members reduces isolation and provides emotional relief. Support circles, whether in person or online, connect women with others who understand the journey. Hearing similar stories normalizes challenges and offers encouragement. It’s important to seek connection without waiting to “feel ready”—vulnerability itself can be healing. Talking about setbacks, fears, or small victories builds resilience. Emotional healing doesn’t require dramatic interventions; it grows through daily acts of awareness, expression, and connection.
Staying on Track: Building a Sustainable Routine
Consistency is the cornerstone of recovery, but it doesn’t come from willpower alone—it comes from integration. The most effective rehab routines are not separate from daily life but woven into it. Linking movement to existing habits increases adherence. For example, doing gentle stretches after brushing teeth in the morning or practicing deep breathing while waiting for the kettle to boil creates natural cues. Pairing strength exercises with a favorite podcast or audiobook makes the time enjoyable. The goal is to make recovery practices feel less like obligations and more like self-care rituals.
A realistic weekly plan balances activity and rest. A sample schedule might include light walking five days a week, two sessions of supported strength work, and daily breathing or mobility exercises. Rest days are not omissions but intentional parts of the plan—times for the body to repair and integrate gains. Flexibility is key; adjusting the plan based on energy levels prevents burnout. On high-energy days, it’s tempting to do more, but overexertion often leads to setbacks. On low-energy days, even five minutes of mindful movement counts as progress. The focus remains on showing up, not performing.
Common setbacks include overdoing it after a good day or quitting after a bad one. To avoid this, set process-based goals rather than outcome-based ones. Instead of “walk 30 minutes,” aim for “step outside and move for 10 minutes.” This approach reduces pressure and builds momentum. Tracking progress through a simple log—marking days of movement, noting energy levels, or listing one positive moment—provides visual feedback and motivation. Over time, these small, consistent actions accumulate into meaningful change. Recovery is not a sprint or even a marathon—it’s a series of daily choices that honor the body’s need for time, care, and patience.
True rehabilitation isn’t about rushing back to “normal”—it’s about building a stronger, wiser version of yourself. For women, this means honoring unique needs, moving with intention, and embracing recovery as a form of self-respect. The journey isn’t always fast, but every small step counts. With the right approach, healing becomes not just possible—but empowering.